EMDR
EMDR stands for Eye Movement Desensitization and Reprocessing. EMDR is used within a comprehensive treatment plan to promote recovery from identified difficulties and past traumas.
EMDR emphasizes the brain’s natural ability to heal.

EMDR as an Integration of Neuroscience, Psychology, and Holistic Approach to Healing
By facilitating neural connections, calming the amygdala, enhancing the Prefrontal Cortex’s regulatory functions, supporting sensory integration, interoceptive awareness, and modulating the Brain's Default Mode Network (DMN), EMDR enables the brain to process and resolve traumatic memories effectively. It represents a convergence of psychology and neuroscience, creating lasting changes in how clients experience and relate to their past.
EMDR introduces a Healing process that is an activation of your brain's natural ability to heal psychologically, just as your body does with a physical wound. We are wired to heal and achieve equilibrium. EMDR can accelerate therapy by resolving the impact of your past traumas and allowing you to live more fully in the present as an active participant in your life. This treatment approach, which targets past experience, current triggers, and future potential challenges, results in the alleviation of presenting symptoms, a decrease or elimination of distress from the disturbing memory, improved view of the self, relief from bodily disturbance, and resolution of present and future anticipated triggers.
EMDR’s capacity to process trauma both verbally and nonverbally makes it a uniquely holistic approach to therapy. By engaging the brain and body in ways that don’t rely on words alone, EMDR honors the full range of human experience, acknowledging that healing can happen even in silence. This nonverbal dimension allows trauma to be addressed at its core, empowering individuals to resolve distress at a sensory, emotional, and physiological level, fostering true and lasting healing. EMDR accesses the inner healer and harnesses the brain’s natural capacity for healing, offering a transformative path toward relief, integration, and well-being.

Reprocessing Trauma, Stimulation, and Memories in a Regulated State
EMDR is particularly effective in helping the nervous system adopt a regulated, calm state during reprocessing. By creating a “safe enough” environment, EMDR enables individuals to revisit traumatic memories without triggering intense survival responses. This safe processing is crucial, as it allows the Prefrontal Cortex (responsible for emotional regulation and executive function) to reconnect with the Hippocampus, which is essential for contextualizing memories. Together, these regions work to defuse the heightened emotional charge, making memories less fragmented, less activated in the body, and more accessible from a rational perspective. This co-regulation between brain areas facilitates a shift in how trauma is stored and recalled, allowing the brain to recognize these events as past occurrences rather than present dangers.
-
Traumatic experiences are often stored as implicit memories—wordless, sensory-laden impressions that the brain holds in a state of high emotional reactivity. EMDR’s bilateral stimulation enables these implicit memories to transition into explicit memories, meaning they can be verbally expressed, understood, and placed within a coherent narrative. This shift is profound, as it helps experience a sense of closure and integration. Traumatic memories that once felt immediate and overpowering can now be recalled without activating survival responses. Instead of lingering as unresolved distress, these memories become part of a personal story that can be revisited with understanding and emotional distance.
-
Through the repeated processing cycles in EMDR, the brain and body learn to release habitual survival responses associated with trauma. EMDR encourages the nervous system to recognize that sympathetic activation (fight/flight) or dorsal vagal shutdown (freeze) is no longer necessary. Over time, the brain builds a capacity to return to a ventral vagal state—a condition of feeling safe, calm, and socially engaged. This shift impacts the Amygdala, which is responsible for detecting threats and generating emotional responses. EMDR reduces hyperarousal in the Amygdala, dampening its immediate reactions to traumatic memories and allowing the brain to shift out of survival mode.
-
One of the transformative aspects of EMDR is its capacity to process trauma beyond words. Many traumatic experiences are stored as sensory and emotional impressions, which are often inaccessible through verbal recall alone. For many people, especially those who have experienced complex or preverbal trauma (trauma occurring before language development), EMDR’s nonverbal aspect offers a pathway to healing without requiring detailed storytelling. It allows clients to work with the sensory and emotional components of trauma without reliving or articulating every detail. EMDR facilitates nonverbal processing by engaging implicit memory systems—those parts of the brain that hold visceral, wordless memories of traumatic events. This can make EMDR an especially accessible and less re-traumatizing form of therapy for those who feel overwhelmed or disempowered by traditional talk therapy.
-
Traumatic memories can become “stuck” as implicit memories, held in the body as sensations, images, and emotional charges rather than as coherent narratives. EMDR bypasses the need for detailed verbal descriptions, allowing clients to reprocess trauma at a fundamental, sensory level. By activating both hemispheres of the brain through bilateral stimulation, EMDR taps into these implicit memory networks, enabling clients to experience shifts in body sensations, emotional states, and mental images without needing to articulate them verbally. This makes EMDR especially valuable for those who struggle to put their experiences into words—whether due to the nature of their trauma, cultural factors, developmental history, or individual neurodivergence.
-
EMDR’s nonverbal approach integrates the body’s responses directly into the therapeutic process. As clients move through the bilateral stimulation sets, they often become aware of shifts in body sensations, such as tension releasing from muscles or a newfound feeling of groundedness. These sensations are integral to processing trauma because the body often “remembers” experiences the mind cannot consciously access. Through this process, clients are invited to notice and experience these sensations without needing to rationalize or verbally analyze them. This somatic, nonverbal processing fosters deeper integration, as trauma is released not only from cognitive but also from physiological pathways.
-
EMDR process is not just about processing the traumatic memories; it is also about reinforcing and accessing positive experiences and resourcing. Before diving into traumatic memories, therapists help clients access safety/ safe enoughness, build trust, and identify positive memories and sensations. This 'resourcing' process strengthens positive neural networks. Resourcing may Include mindfulness, grounding, meditation, breathwork, guided imagery, positive memory recall, somatic practice, sensory awareness, music, movement, play, creativity, and other types of soothing and regulating activities and practices that resonate personally to support nervous system regulation and access positive neural networks in the brain. When mindfulness and resourcing are practiced positive neural networks in the brain are strengthened, making them more accessible during EMDR. Mindfulness-based resourcing supports the emotional strength and tools needed to handle whatever comes up during the EMDR process.
-
By engaging in verbal and/or nonverbal processing, EMDR helps clients develop a compassionate relationship with their body and nervous system. Clients learn to observe their internal experiences like muscle tightness, tingling, warmth, or shifts in breathing as meaningful signals from the body that support emotional processing. Over time, this body-based awareness empowers clients to trust their own physical sensations and internal cues, recognizing them as allies in the healing process.

Neuroplasticity and Long-Term Healing
Neuroplasiticity, the brain’s ability to reorganize and form new neural connections, is central to EMDR’s effectiveness. Each EMDR session serves as a catalyst for rewiring the brain, transforming traumatic memories into experiences that no longer trigger high emotional reactivity. Through this process, people achieve lasting relief and a greater capacity for emotional regulation, demonstrating the brain’s remarkable ability to heal and adapt.

How EMDR Modulates Core Brain Regions impacted by Trauma
TLDR:
Downregulating the Amygdala and HPA Axis
Bilateral stimulation reduces overactivation of the amygdala, telling the nervous system “you are not in danger right now.” Cortisol and adrenaline output decrease, shifting the body into a parasympathetic state of rest, digestion, and repair.
Re-engaging Cognitive Control and Body Awareness
EMDR activates the ACC and insula, bringing back online the capacity to notice body signals, regulate, and reframe experiences. Clients often describe this as “finding words for what I feel” or “being able to stay present without being overwhelmed.”
Balancing Brain Networks
EMDR interrupts DMN dominance, quiets shame and intrusive loops, supports nervous system regulation, and strengthens the TPN and salience networks. The result is increased clarity, present-moment orientation, and an empowered sense of choice.
Cross-Hemispheric Integration
EMDR promotes communication between brain regions by establishing “neuro-fiber bridges” along the Corpus Callosum, a thick bundle of nerve fibers that connects the brain's hemispheres. By engaging the corpus callosum, EMDR enables both sides of the brain to work together: the right brain’s emotional and sensory experiences can connect with the left brain’s language, reasoning, context, and narrative. This bridge allows memories to move fluidly across regions, transforming trauma from fragmented, isolated memories into cohesive narratives and integrated memory that no longer feels threatening.
-
The amygdala is the alarm bell of the brain, involved in fear and threat detection. It asks the question, “is this dangerous?” It is important in helping to survive when there is actual danger or threat and it prunes itself to the environment. When it becomes overactive, it causes the nervous system stuck in high alert. This overactivation sends constant “fight, flight, freeze, or fawn” signals and floods the body with stress chemicals, even when no present-day threat exists.
-
The hippocampus is like the long term storage unit responsible for learning memory, explicit, declarative, autobiographical memory. The hippocampus is what places experiences in time, sequence, and context, so you know what happened first, what came after, and that something belongs to the past rather than the present.
When trauma happens, this function gets disrupted. Memories can be stored in fragments, body sensations, or raw sensory impressions instead of a coherent storyline. Flashbacks or intrusive memories feel like they’re happening right now because the hippocampus has lost its ability to anchor them in time.
The hippocampus is also covered in cortisol receptors. When trauma is intense or ongoing, those receptors get flooded by stress hormones. Too much cortisol can impair the hippocampus, making it harder to encode and retrieve memory accurately. That’s why in complex trauma, memories may feel blurry, missing, or scrambled, while the body still holds onto the intensity of the experience.
The hippocampus also has a regulating relationship with the amygdala, acting similar to an air conditioner. Normally, the hippocampus helps calm it down by cross-checking with memory: “This looks similar, but it isn’t the same thing. You’re safe now.”
But when the hippocampus is dysregulated, that communication breaks down. Instead of sending a calming signal, it may send a generalized danger cue.
The amygdala asks: “Is this dangerous?”
A healthy hippocampus responds: “No, this is just a reminder, not a threat.”
A dysregulated hippocampus may respond: “Yes, this is the same as before! Sound the alarm!”
This is how trauma creates false alarms, where the body and nervous system react to present-day triggers as if the original danger is happening again.
EMDR helps the hippocampus come back online. Through bilateral stimulation and reprocessing, the hippocampus can re-anchor traumatic memories in their proper time and place, telling the amygdala: “That was then, this is now.” This shift allows memories to be integrated into the broader life story, no longer overwhelming or frozen, but part of a larger narrative that the nervous system can hold with more clarity and regulation.
-
The hypothalamus communicates directly with the pituitary gland and adrenal glands (the HPA axis), setting off cascades of stress hormones, cortisol and adrenaline. Chronic trauma and stress dysregulates this system, resulting in either constant revved up hyperarousal, constantly flooding the system, or burned out, exhausted, and blunted. This is why trauma survivors may experience the feeling that their bodies are betraying them, swinging between hyperactivation and collapse.
-
The ACC is like the inner “bridge” of self-regulation. It is a cortical brain region involved in cognitive control, self-regulation, error detection, and conflict monitoring. When trauma and stress, and worry dominate, the ACC goes offline. That means that there is no ability to pause, reflect, regulate emotion, redirect attention, and feel a sense of control in the present. When the AAC is offline, it contributes to a defaulted sense of “I can’t control this. I’m not really here.”
-
The insula helps us sense the inner world of the body’s felt state (interoception). Supports interoceptive awareness (the ability to sense internal body states). Trauma disrupts insula activity, leading to difficulties noticing or trusting body sensations, a key factor in dissociation or emotional overwhelm. The Insula works directly with the Cingulate to interpret these messages and respond to them.
-
The Default Mode Network (DMN) is a large-scale brain system that turns on when the mind is not engaged in an external task. It’s active during daydreaming, mind-wandering, self-reflection, and imagining possibilities. In a balanced state, the DMN is not harmful.
In trauma, the DMN loops on cycles of negative self-beliefs, intrusive memories, and shame spirals, instead of fluid thought exploration.
When the DMN dominates due to stress, depression, anxiety, or trauma, the anterior cingulate cortex (ACC) and other regulation hubs go offline. This is why it feels impossible to pause, reorient, to calm down, or to feel present. This overactive self reflection gets stuck in looping in old narratives or catastrophized self-referenced “conspiracy theories” and unable to regulate.
The DMN also works in tension with the Task Positive Network (TPN), which activates when we are engaged, task-focused, and present. Trauma overloads the DMN and silences the TPN, keeping thoughts trapped in the “inner loop” rather than anchored in the now and able to redirect.
EMDR helps rebalance the DMN by interrupting stuck DMN cycles and bringing the ACC and insula back online, allowing for self-awareness, regulation, and the ability to sense the present. Instead of being snatched into shame spirals or dissociation, the DMN can return to its healthy functions: creativity, reflection, and integration.
-
The Task Positive Network (TPN) is the brain’s “here-and-now network” made up of several regions working together, including the AAC and Insula. It switches on when we are task-focused, present, and actively engaged in goal-directed tasks. EMDR helps shift activation out of the DMN and into the TPN, supporting access to present-moment processing, problem-solving, and flexible attention.
EMDR engages the TPN directly. Bilateral stimulation shifts activation out of DMN loops and into TPN pathways, reawakening the ACC and insula so clients can:
Notice and regulate body states without overwhelm
Focus attention long enough to reprocess memories
Make decisions and access choice in the present moment
Anchor themselves in safe-enoughness while working on processing difficult memories, emotions, thoughts, and felt states
This is the mechanism that allows traumatic experiences to be processed without the system becoming flooded. The ACC comes back online to guide regulation, the insula reconnects sensation with meaning, and the TPN keeps attention grounded in the here-and-now.
-
The salience network (SN) is a brain system responsible for coordinating the brain’s resources necessary for determining what is important to pay attention to, both inside the body and outside in the environment.
It includes key nodes such as the Anterior Insula and Dorsal Anterior Cingulate Cortex. This helps the brain respond to changing demands by moderating neural networks.
Trauma skews it toward hypervigilance, resulting in every cue feeling like danger because the salience network sends exaggerated signals to the amygdala and DMN, reinforcing hypervigilance, intrusive memories, or dissociation. This feels like the nervous system being constantly on guard or “waiting for the other shoe to drop.”
EMDR helps rebalance the salience network so the system can detect cues of safety as well as threat, which is key to nervous system recalibration. The salience network learns to tag safety cues as relevant again not just danger as relevant. This shift is critical because it tells the body and brain that connection, regulation, calm, rest, and choice are worth paying attention to in order to exist.
-
The corpus callosum is the brain’s great neurofiber bridge, connecting the left and right cerebral hemispheres through approximately 200 million to 300 million axons, myelinated nerve fibers. It allows information to flow between the hemispheres so that thinking, feeling, sensing, and remembering can come together as one coherent experience.
In trauma, this bridge often gets backed up, like a traffic jam at rush hour. Signals pile up in the midbrain and can’t make it across. This is why traumatic memories often feel fragmented, either an overwhelming body flash with no words, or a detached story with no felt connection. The traffic is stuck.
Sometimes the traffic jam is so bad that detours happen, like dissociation, hypervigilance, or numbness. The nervous system finds ways to cope, but the cost is disconnection.
EMDR works like a traffic controller on this highway, ensuring a safer navigation towards a healing destination. Bilateral stimulation signals left-right-left-right, opening the lanes of the corpus callosum and allowing information to cross again. Slowly, the traffic jam clears, lanes reopen, traffic flows, integration happens. Memories can move into long-term storage as part of a coherent life story rather than staying stuck in the present.
This bridge allows the Neocortex to calm the emotional responses of the Limbic System, allowing for the space to make sense of these memories and felt states within a larger life context.
Neurons establishing new connections via neuroplasticity
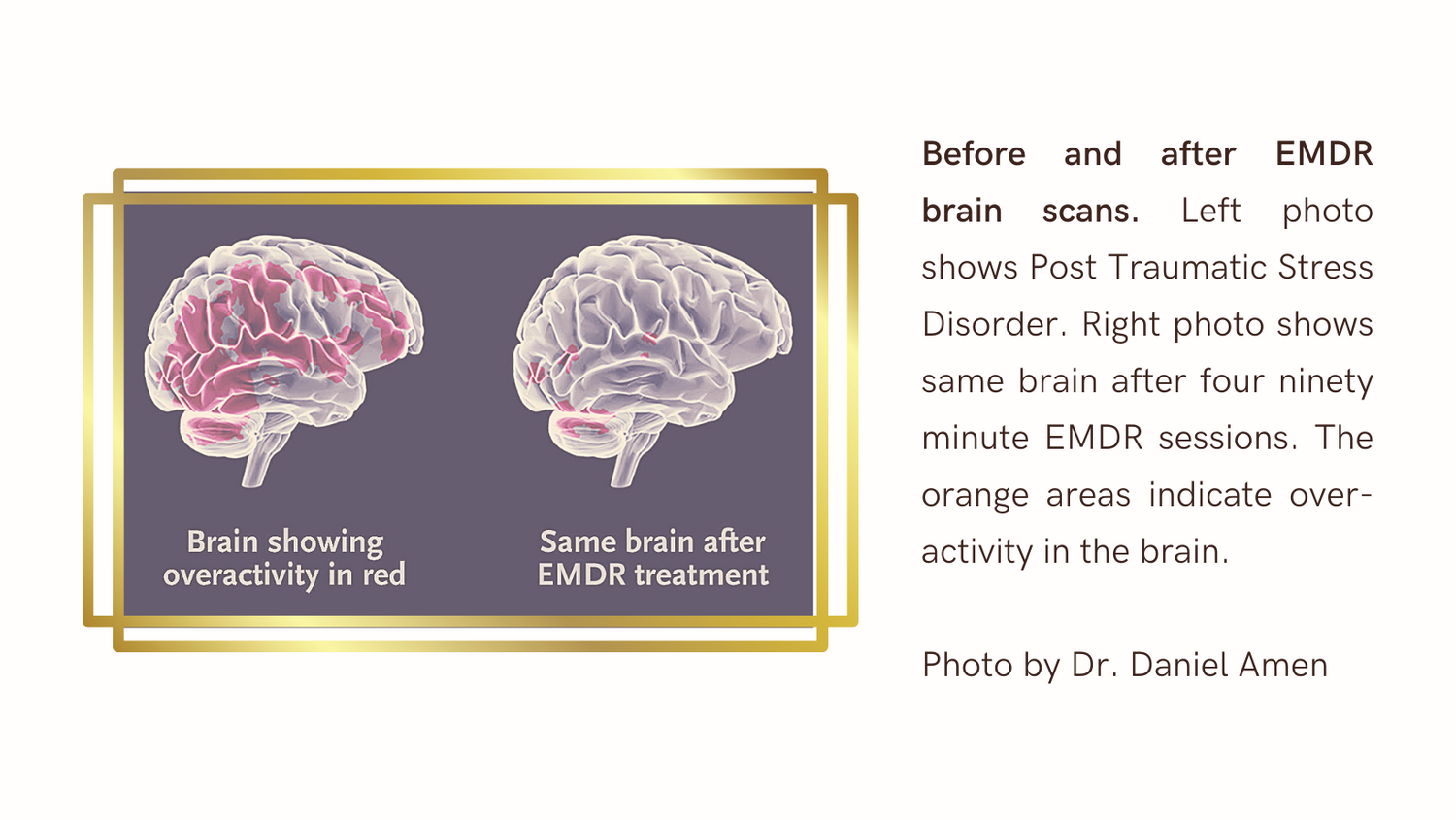
Brain Imaging Studies
Brain research has shown that trauma significantly alters not only brain chemistry, but also brain structure; PET brain scans have shown that EMDR facilitates neurobiological repair. Reduced amygdala hyperactivity and increased hippocampal activity post-EMDR suggest effective memory reprocessing.
Through neural shifts, EMDR creates:
Safety and calm: the nervous system learns it is not in immediate danger.
Integration: fragmented memories become whole, with context and perspective, and no longer disturbing.
Resilience: new positive neural pathways strengthen future responses to stress.
Empowerment: reclaim choice, self-compassion, and clarity, instead of being pulled back into old trauma-driven reactions

Bilateral Stimulation & Dual Attention
Bilateral Stimulation (BLS)
Bilateral stimulation is central to Eye Movement Desensitization and Reprocessing (EMDR) therapy. It mirrors the brain’s natural process during REM (Rapid Eye Movement) sleep, where the brain processes daily events and makes sense of unconscious material. In EMDR, we replicate this process to help the brain reprocess memories and felt states.
Dual Attention Stimulus (DAS)
Dual Attention Stimulus (DAS) is another essential component of EMDR. It involves holding two things in mind simultaneously:
The Traumatic Memory (or distressing/activating material/target).
An External Stimulus that alternates between left and right (bilateral).
This combination of focusing on both the memory and an external stimulus helps the brain reprocess the memory in a way that reduces its emotional intensity.
-
Bilateral stimulation involves stimulating both hemispheres of the brain alternately. This can be done in several ways:
Eye Movements: Moving the eyes back and forth by following a therapist’s hand or an object.
Tactile Stimulation: Alternating tapping on the shoulders, knees, or hands, or tossing a ball from one hand to the other.
Auditory Stimulation: Listening to alternating tones in each ear.
This left-right stimulation engages the brain in a way that promotes adaptive information processing, helping the brain to reorganize distressing memories so they can be recognized without the intense emotional charge.
-
The dual attention and bilateral stimulation techniques together engage both hemispheres of the brain. This balanced, simultaneous engagement supports:
Brain Integration: Traumatic memories are stored in an isolated manner, meaning they're not integrated with other memories and can continue to trigger distress. By maintaining attention on both the traumatic memory and the bilateral stimulus, DAS facilitates the brain’s processing of distressing memories. This allows the memory to be integrated in a healthier, less distressing way. This 'back and forth' activity encourages the brain to process and reorganize these traumatic memories and negative thoughts, so they're integrated into a person's life story and stored in the brain adaptively without the same distress.
Promoting Relaxation: It activates the parasympathetic nervous system, providing a calming effect and making it safer to process traumatic memories.
Reduces Emotional Charge: Helps the brain process the trauma without the same level of distress, allowing for a more adaptive perspective on the memory.
-
Once positive neural networks are identified through resourcing, bilateral stimulation can be used to strengthen neural connections and reinforce regulating nervous system connections. By linking the positive sensations with the bilateral stimulation, the client can access these positive networks even when discussing or recalling distressing memories and felt states. The constant engagement of both brain hemispheres through the bilateral stimulation method helps in soothing and reprocessing traumatic memories with the presence of these positive associations.
-
he Process
Stimulation Period: Bilateral stimulation is applied briefly and then paused.
Feedback and Reflection: After pausing, the client provides feedback about their experiences, such as changing thoughts, images, or feelings. It's essential for the client to offer genuine feedback without judgment.
Adaptive Processing: The therapist guides the client through a series of repeated sets of bilateral stimulation, combined with breathing, body scanning, noticing, and sharing. This method helps to process and reorganize traumatic memories, making them less intense.
EMDR Protocols are modified to facilitate healing and support adaptive processing, sensory needs, nervous system regulation, accessibility, safety, and the unique needs of each client.
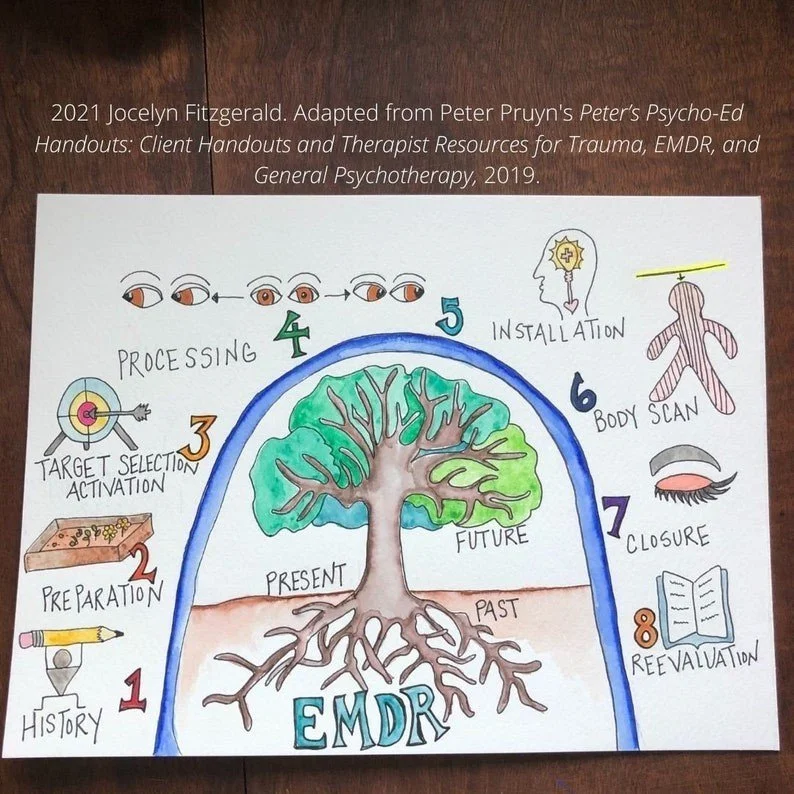
The Standard EMDR Protocol Integrates an 8 Phase Approach
-
Together, we will discuss your current challenges and symptoms, when they are most noticeable and problematic, what your hopes and goals are for the future, and some background information.
-
Components:
Safety (or safe enough-ness) in our therapeutic space - Before any EMDR starts, I make sure that we have a foundation that feels strong, trusting, and aligned.
Education – we will discuss EMDR and make sure that I have adequately responded to your questions. I encourage you to learn about EMDR so that you can make an informed choice about this treatment option and consider ways to maximize its use for your healing and well-being.
Resource Installation – You will be invited to learn and practice mindfulness and regulating techniques to support your nervous system. This may include guided imagery in sessions for visualizing positive peaceful places, people, memories, past successes, and inner strengths, sensory soothing, somatic techniques, and expressive arts, while using bilateral stimulation (eye movements/ tactile bilateral stimulation /auditory tones). These exercises will enhance your ability to comfort yourself when distressed, elevate your mood, empower choice, increase your awareness, release judgment, embrace pace, regulate your emotional responses, and invite your body/mind/spirit into a more relaxed, present state.
Trauma Targeting Plan - Together we will create a list of EMDR “targets.” These are things that cause you upset in your present life including: traumatic memories, negative thoughts, fear/anxiety, symptoms and other distressing feelings, uncomfortable or painful body sensations, disturbing dreams, and current difficult life experiences.
In EMDR, the 'target' can be:Past experiences where you did not perform as well as you hoped to or as expected by others
Life experiences that lessened your confidence
Past negative messages
Current symptoms and feelings that prevent you from focusing
Should/Must statements
Attachment wounds
Memories that feel blank or fragmented
Ableism / Internalized Ableism
Negative Beliefs
Pre-verbal trauma
Specific Phobias/Anxieties
Non-ordinary states / expanded states of consciousness
Specific Trauma
Any other barriers that keep your from working/performing/living up to your potential
-
At this phase you will choose a safe word for the processing session that can be used if you want the EMDR to stop or pause. This can be any word besides “no” or “stop”
Example safe words: giraffe, ketchup, goat, tourmaline, potato
We will then choose the “target” you would like to work on/get relief from. You will be asked about what the worst part of that target memory is, what image is represented by it that flashes in your head, what thoughts, feelings, and body sensations go with it, and what it makes you believe about yourself now.Then you till be asked to rate the distress it causes on a scale from 0-10.
You will also be asked what you would like to believe about yourself instead.
Then you will be asked to rate how true that currently feels on a scale from 1-7. This will help us measure where we are in the process.
-
You will be asked to bring up the target you have chosen, along with the disturbing image that represents it, the negative belief you have about yourself as a result of it, and the distressing feelings and body sensations it still evokes for you. This activates the neural networks in your brain where the trauma is stored so that it can be “unlocked” and processed. I will then add the bilateral stimulation (eye movements, tapping, gentle buzzing in your hands, auditory tones).
After reprocessing, the goal is that you will be able to recall or notice the upsetting memory with a distress rating of 0 or a humble 1 and your positive belief at a rating of 7 or a humble 6. It does NOT mean that the distress you felt at the time of the event changed; that cannot ever be changed. It means that your body and mind have transformed it into a memory that happened in the past and it no longer feels like an experience happening now. Desensitization then continues by targeting current triggers (things in the present that are upsetting) as well as anticipated future triggers and rehearsing addressing them effectively.
-
When the target memory has been desensitized (the distress level is 0-1 on a scale of 0-10 and the positive belief is 7 on a scale of 1-7) we will link the positive belief to the target memory using the bilateral stimulation.
-
You will be asked to hold the target in your mind along with the positive belief, and to mentally scan your body from head to toe. If you notice any tension or tightness or discomfort we will add additional bilateral stimulation until the discomfort is gone or reduced. When you notice positive sensations, we will add bilateral stimulation to strengthen and enhance them.
-
After every session it is my intention to hold space for your process to unfold and to support you in leaving sessions feeling safer, seen, empowered, and grounded. If we are in the middle of reprocessing a negative memory but the session time is about to end, I will lead you in a relaxation exercise and help connect you to your positive resources.
-
The next time we meet we will discuss what you have experienced since your last session. I will ask you to bring up the original target and make sure the positive changes have remained. Once the target has been fully processed we will use bilateral stimulation for future performance improvement and strengths enhancement.
-
EMDR facilitates deep and lasting changes. During an EMDR session your mind will move quickly from one memory/scene to the next to the next; this process will continue between sessions as your mind-bodyspirit continue to move toward healing.
It is NORMAL for people to discover new information, make unexpected connections, and to experience strong positive as well as strong negative emotions between sessions. It is also normal for the changes to be more subtle and gradual.
Usually unexpected positive resources also spontaneously come to mind or in dreams. I encourage you to spend time between sessions practicing and strengthening the neural connections of the positive resources you have developed. Most people find this a very pleasurable, empowering, and comforting part of EMDR.
It can be helpful to write down or artistically express what happens for you between sessions in your own journal/sketch book and use the TICES log journal that will be available in your client portal.

What Does EMDR Reprocessing/Desensitization Feel Like?
People have different experiences of EMDR. Some say it is like rapid daydreaming; some describe it as watching scenery go by from the window of a train; others liken it to watching a movie or snapshots in a slide show; some compare it to prayer, active daydreaming, or meditation. Most people have commented that it is like going into a painful memory and bringing along the sensation of comfort, like being rocked and soothed when distressed. Sometimes people cry, releasing strong emotions and sometimes people experience physical sensations as their body releases its sensory experiences. You ALWAYS remain in control and able to stop, ask questions, or obtain my help in figuring out and getting what you need. You ALWAYS have consent and access to your safe word or safety signal that we will both know.
Unlike exposure therapy, the experience of EMDR is NOT a moment-by moment reliving of a painful life event; instead the traumatic memory links up with positive, useful information and resources that are also stored in your brain. EMDR creates “dual awareness” which means that instead of getting fully pulled into a memory, the bilateral stimulation supports regulation and integration of difficult parts of the process.
EMDR does not make people forget their painful experiences or stop being sad sometimes about them; however the memories will become just that: memories. They will become less upsetting because they will be filed in the brain as something that happened in the past instead of being relived over and over in the present; you will be able to recall them but without the painful emotional charge.
Because the part of the brain that communicates in images works faster than the part of the brain that communicates in words I will encourage you to talk less than traditional therapy. After each set of bilateral stimulation you will be asked what you are noticing or what you are present to, and your answer is honest feedback, even if it is unrelated or your mind wandered. There is no wrong way to do this. You will then be told to “go with that” or"notice that" or "stay with that." If at any time you feel overwhelmed or “stuck,” I will be right here with you to support, offering gentle prompting, pacing, reminders, guidance, bilateral stimulation, and co-regulation. There are many things I can do to help.
EMDR works by enhancing your body’s own natural healing processes. It is your brain’s neural networks and channels of associations that control the EMDR desensitization process. The bilateral stimulation simply helps you move your own eyes, tactile movements, and awareness back and forth across the midline of your body so that the hemispheres of your brain talk to each other more efficiently.
YOU CANNOT DO EMDR WRONG; everyone’s process is wonderfully unique.
In your online EMDR session, you will be introduced to tapping, auditory, and visual bilateral stimulation via an online platform called BilateralBase

Credibility - Does EMDR Really Work?
Eye Movement Desensitization and Reprocessing (EMDR) therapy EMDR is an extensively researched, structured, and effective mind-body psychotherapy method that is internationally recognized as an empirically supported treatment when provided by a clinician who has completed an EDMRIA Approved Training in EMDR. www.emdria.org
-
Ableism/ Internalized Ableism
Addictive Behaviors
Adjustment
Anger
Anxiety
Attachment
Burnout
Chronic Pain/Illness
Complex Trauma
Compulsions
Creativity-“Flow” Development
Cultural experience
Dependency
Depression and other mood disorders
Dissociation
Emotional eating
Experiences/Memories that are painful to recall
Identity
Imposter Syndrom
Integration of expanded or non-ordinary states of consciousness
Loss and Grief
Medical Trauma
Neurodivergent Burnout
Pain reduction
Phobia
Perfectionism
Performance enhancement: athletic/academic/musical/professional/general
Procrastination/avoidance behaviors/indecision
Racial Trauma
Relationship enrichment/healing
Rejection Sensitive Dysphoria (RSD)
Self-esteem improvement
Stress management
Trauma
-
NY Times: The Evidence of EMDR
NY Times: Expert answers on EMDR
The practice guidelines of the American Psychiatric Association (2004), American Psychological Association, & the Department of Veterans Affairs and Defense (2004) have placed EMDR in the highest category of effectiveness. You can read more specific research citations and information at EMDRIA.
EMDR is currently a top rated treatment for trauma, both single incident (car accident, natural disasters) and complex (chronic childhood deprivation and abuse).
If you would like to read more about EMDR, including case studies, I recommend:
EMDR: The Breakthrough “Eye Movement” Therapy for Overcoming Anxiety, Stress, and Trauma by Francine Shapiro & Margot Silk Forrest
Getting Past Your Past: Take Control of Your Life With Self-Help Techniques From EMDR Therapy by Dr. Francine Shapiro
EMDR Essentials: A Guide for Clients and Therapists by Barb Mailberger
-
-
Clinical Resource Efficiency Support Team (CREST) of the Northern Ireland Department of Health
Dutch National Steering Committee for Health Care
French Haute Autorite de Sante (French National Authority for Health)
French National Institute of Health and Medical Research (INSERM)
Israeli National Council for Mental Health
The Rail Safety and Standards Board, United Kingdom
The Trimbos Instituut, The Netherlands
United Kingdom National Health Service (NHS)
United Kingdom Psychological Trauma Society
United States National Alliance on Mental Illness (NAMI)
Other international health and governmental agencies
EMDRIA EMDR Intro Video
Jameela Jamil opens up about what healing has looked like after experiencing abuse in childhood, and how EMDR has helped her process and move through trauma.
Actress AnnaLynne McCord shares her emotional and physical Experience of EMDR and how it helped her heal and understand her dissociative identity disorder diagnosis, traumatic memories, self harm, black outs, panic, burning sensations, and her body moving around involuntarily.
An In Person EMDR demonstration with finger tracking eye movements for bilateral stimulation by Dr. Jamie Marich - Expert EMDR trainer, author, and founder of Institute fro Creative Mindfulness
Sandra Bullock’s EMDR experience, with paddles Bilateral Stimulation
EMDR Therapy Demonstration and step-by-step walk through breaking down his recorded experience of EMDR - by The Chocolate Therapist
Lil Jon Reveals How EMDR Therapy Unlocked Hidden Childhood Trauma
A virtual EMDR demonstration session with a metronome and tapping for bilateral stimulation - from Institute fro Creative Mindfulness, with Paula Lavocat and Blaise Harris
A scene from Uptown Girls that beautifully depicts what EMDR Therapy Feels Like when working with healing inner child parts of self
Scenes from Greys Anatomy showing Dr. Jo Wilson experiencing EMDR processing with target image identification, negative cognition, BLS, flashbacks, positive cognitions, resourcing, and support from her therapist.
Prince Harry's EMDR experience, with tapping Bilateral Stimulation
Miley Cyrus credits EMDR therapy for saving her life, curing her stage fright and allowing her to finally let go of the anxiety of wanting everyone to love her.